What is Pelvic Girdle Pain (PGP)?
A Physiotherapist’s Guide
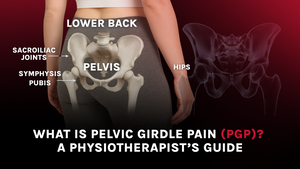
Pelvic girdle pain (PGP), also known as symphysis pubis dysfunction (SPD), is discomfort occurring in the front and/or back of the pelvis, including the sacroiliac joints and the symphysis pubis joint. It's a common condition, particularly during pregnancy, and can significantly impact mobility and quality of life (Vleeming et al., 2008).
Understanding Pelvic Girdle Pain (PGP): What It Is and How It Affects You
What Is Pelvic Girdle Pain?
PGP refers to pain experienced in the pelvic region, including the symphysis pubis at the front, the sacroiliac joints at the back, and surrounding areas such as the hips, lower back, and thighs. It’s often worsened by weight-bearing activities and can persist after childbirth (Kanakaris et al., 2011).
Why Does PGP Happen?
The pelvis comprises three main joints: one symphysis pubis joint at the front and two sacroiliac joints at the back. These joints normally work in unison to provide both stability and movement. In cases of PGP, they may move unevenly or become unstable, causing pain and functional issues (O’Sullivan & Beales, 2007).
During pregnancy, several factors contribute to PGP, including:
-
Hormonal changes (particularly relaxin) that increase ligament laxity.
-
Additional weight and biomechanical stress placed on the pelvis.
-
Previous injuries to the lower back or pelvis.
-
Hypermobility or generalized joint instability.
Common Symptoms of PGP
PGP symptoms vary but may include:
-
Pain in the pubic bone, hips, groin, lower back, or thighs.
-
Pain worsening with walking, climbing stairs, or turning in bed.
- Clicking, grinding, or an unstable sensation in the pelvic area.
These symptoms can be debilitating, limiting daily function and affecting sleep and emotional well-being (Verstraete et al., 2013).
How PGP Affects Daily Life
For many, PGP interferes with routine activities—walking, standing, lifting, and even rolling over in bed may become painful. Left unaddressed, it can increase the risk of chronic pain and postpartum complications (Elden et al., 2008).
How Supacore Can Help?
Supporting Pelvic Stability Where It Matters Most
Supacore’s patented Coretech® technology is designed to mimic the body’s deep core muscles, offering medical-grade compression to the pelvic region. The targeted compression stabilizes the pelvis and reduces asymmetrical joint movement, easing strain on the sacroiliac joints and pubic symphysis (Ghanbari et al., 2018).
Real Relief from Real Pain
PGP often flares during everyday motions. Supacore’s compression helps reduce pain and promote alignment, offering support that adapts to movement. Benefits include:
-
Reduced lower back and hip pain.
-
Relief from groin pressure and pelvic instability.
- Minimized pain during walking or climbing stairs.
This can help improve function without the bulk or rigidity of traditional pelvic belts (Mens et al., 2006).
Encouraging Muscle Engagement and Body Awareness
Beyond structural support, compression also improves proprioception—your body’s ability to sense its position. This leads to better neuromuscular control, activating stabilizing muscles like the pelvic floor and transverse abdominis (MacRae et al., 2011). Improved proprioception can lead to:
-
Better postural control.
-
Reduced compensatory movement.
- Decreased risk of long-term dysfunction.
Ideal for Postpartum Recovery Too
Pelvic instability often lingers post-birth. Supacore garments continue to provide support during postpartum recovery by:
-
Re-aligning the pelvis.
-
Reactivating deep core muscles.
-
Enhancing movement control and healing.
Studies show that postpartum compression can help women regain stability and manage pain more effectively (Elden et al., 2008).
Comfort Meets Clinical Integrity
Supacore maternity and recovery garments are:
-
Seamless and body-mapped for everyday wear.
-
Anti-chafing and breathable.
-
Clinically tested for durability (up to 150 washes).
-
Sustainable and ethically made.
In Australia, Supacore garments may qualify for private health rebates, making clinically-informed support more accessible.
A Smarter Way to Support Your Pregnancy
You don’t have to tolerate pelvic pain. Supacore’s Coretech® compression is based on clinical insight and designed for real women’s lives. It’s more than just a product—it’s a solution built to support your journey through pregnancy, recovery, and beyond.
References (APA Style)
Albert, H., Godskesen, M., & Westergaard, J. G. (2002). Evaluation of clinical tests used in classification procedures in pregnancy-related pelvic joint pain. European Spine Journal, 11(6), 482–488. https://doi.org/10.1007/s00586-002-0467-5
Elden, H., Lundgren, I., Robertson, E., & Olsen, M. F. (2008). Effects of acupuncture and stabilising exercises as adjunct to standard treatment in pregnant women with pelvic girdle pain: Randomised single blind controlled trial. BMJ, 336(7635), 1225–1227. https://doi.org/10.1136/bmj.39563.440329.BE
Ghanbari, A., Moghaddam, A., Jamshidi, A., & Sadeghi-Demneh, E. (2018). The effect of pelvic support belts on pain, disability and pelvic alignment in pregnant women with pelvic girdle pain. Physiotherapy Theory and Practice, 34(9), 697–704. https://doi.org/10.1080/09593985.2018.1438521
Kanakaris, N. K., Roberts, C. S., & Giannoudis, P. V. (2011). Pregnancy-related pelvic girdle pain: An update. BMC Medicine, 9(15). https://doi.org/10.1186/1741-7015-9-15
MacRae, B. A., Cotter, J. D., & Laing, R. M. (2011). Compression garments and exercise: Garment considerations, physiology and performance. Sports Medicine, 41(10), 815–843. https://doi.org/10.2165/11591420-000000000-00000
Mens, J. M. A., Vleeming, A., Snijders, C. J., Koes, B. W., & Stam, H. J. (2006). Reliability and validity of hip adduction strength to measure disease severity in posterior pelvic pain since pregnancy. Spine, 27(15), 1674–1679. https://doi.org/10.1097/01.BRS.0000024345.36123.0F
O’Sullivan, P. B., & Beales, D. J. (2007). Diagnosis and classification of pelvic girdle pain disorders—Part 1: A mechanism based approach within a biopsychosocial framework. Manual Therapy, 12(2), 86–97. https://doi.org/10.1016/j.math.2006.11.005
Verstraete, E. H., Vanderstraeten, G., Parewijck, W., & Van De Velde, G. (2013). Pelvic girdle pain during or after pregnancy: A review of recent evidence and a clinical care path proposal. Facts, Views & Vision in ObGyn, 5(1), 33–43.
Vleeming, A., Albert, H. B., Östgaard, H. C., Sturesson, B., & Stuge, B. (2008). European guidelines for the diagnosis and treatment of pelvic girdle pain. European Spine Journal, 17(6), 794–819. https://doi.org/10.1007/s00586-008-0602-4